We will review 2 clinical scenario interview sample simulations. One has gone well, and the other has gone sideways. This is meant to help you identify what to do and what to avoid during your own interview.
General Surgery Clinical Scenario – Interview done well:
Scenario:
A 75-year-old male patient, who is frail, has dementia, and lives in a nursing home, has been brought to the emergency department. He presents with an acute abdominal pain and signs of sepsis. His blood tests show elevated lactate levels, indicating possible ischemia. His past history further includes: COPD and he is taking clopidogrel. How would you approach managing this patient?
Blood Tests
| Test | Result |
| FHG (Full Haemogram) | Hb: 12 g/dL, WBC: 14 x10^9/L, Platelets: 200 x10^9/L |
| UEC (Urea, Electrolytes, and Creatinine) | Urea: 8 mmol/L, Creatinine: 120 µmol/L, Sodium: 135 mmol/L, Potassium: 4.5 mmol/L |
| LFTs (Liver Function Tests) | AST: 45 U/L, ALT: 50 U/L, ALP: 100 U/L, Bilirubin: 15 µmol/L |
| Coagulation | INR: 1.1, aPTT: 32 seconds |
| Lactate | Lactate: 4.5 mmol/L |
Observations
| Observation | Value |
| Pulse | 110 bpm |
| Blood Pressure | 90/60 mmHg |
| Temperature | 38.5°C |
| Respiratory Rate | 22 breaths/min |
| O2 Saturation | 92% on room air |
Response:
Panellist:
Good afternoon, JW. I’m NJ, an Upper GI surgeon, and I’ve got a colleague of mine, Mr. KK, an emergency general surgeon. So, you’ve read the scenario?
Candidate:
Yes, I did.
Panellist:
Yeah. So what I want you to do is tell us how would you approach managing this patient?
Candidate:
Okay. Thank you for inviting me to this interview.
This patient has several issues, starting from clinical issues, management, and possibly training issues as well. So, in the clinical issues, the patient is 75 years old, is frail, has dementia, and lives in a nursing home, so he probably does not have the mental capacity to be able to make decisions, presenting with acute abdomen and sepsis from the look of his blood, looks to have likely ischemia with lactate that’s elevated, might be having mesenteric ischemia, might be having a perforation or a volvulus that would need surgical management. In terms of the management of this patient, we would need the early involvement of the consultant.
We would need a multidisciplinary approach, including the anaesthesia evaluation to see whether he’s a candidate for surgery, as well as early communication to the theatre in case it’s determined that he needs surgery. We would need to discuss with his next of kin or whoever has legal power of attorney and ultimately make a decision as to whether surgery is appropriate for a patient who is in this kind of state. In terms of training, this presents an opportunity for learning and reflection.
So my initial approach would be to first evaluate the patient, acutely resuscitate the patient, and then move on to take further history, gather more information, and definitively manage the patient. I’d like to organize my team, including the junior medical doctor I’m with, whether that’s a SHO, F1, and make my way to review the patient. I’m going to review the patient using a CCRISP approach, as well as make sure that I’m following the sepsis-6 bundle.
For sepsis-6 bundle, I’ll have to ensure that he’s on high-flow oxygen, paying keynote that he has COPD. I’ll also have to start the patient on IV fluids. He seems dehydrated.
I’ll have to start the patient on IV antibiotics as per the trust policy, ensure we have some urine output monitoring, and some bloods are available but I’d need a blood culture and repeat ABGs and lactate. I’d like to check whether the patient is talking, which would confirm his airway is open. Do the breathing assessment, as mentioned, and in the circulation, ensure he has two large-bore cannulas connected, and bloods taken out.
Further examinations that need to be done that are not included there. I’d like to have a full picture of his ABGs. I’d like to have his LFTs, look at his blood sugar as well, and look at a coagulation profile.
He’s on clopidogrel, so there’s also a need to be able to discuss with haematology later on in case a decision is made for surgery. I’d like to, once the patient is stabilized and started on some medication, I’d like to take a detailed patient’s history and physical evaluation. Of course, the patient might not be able to give me history, so I’d like to get some corroborative history from the carer in the home that he’s in, understand how long he’s been having symptoms, whether he’s been able to pass any stool, how long he’s had any vomiting, the character of the vomit.
I’d also want to understand his compliance to the medications that he’s on. I’d want to understand from a family history and a social point of view, do they have any family history of cancer. In terms of the social aspect, I’d want to know the next of kin and their involvement with him.
I’d also want to objectively grade his frailty from my discussion.
Panellist (interrupts):
And how would you do that?
Candidate:
Okay, so from discussing with the carer, I’d like to know his level of independence. It’s indicated that he’s most of the time in bed, but I’d like to know whether he’s able to get up and move around as well.
Panellist (interrupts):
Yes, so there’s an objective score,
Candidate:
a WHO performance score for frailty. In terms of investigations, I’d want to do a CT abdominal pelvis with contrast. Of course, noting that he may have acute kidney injury as well, which will need to be resuscitated, but his EGFR was at 60, so it’d be fine having a CT abdominal pelvis.
I’d like to discuss or hand over to my SHO to call the radiologist to have this expedited and review the CT scan based on the CT scan findings.
Panellist (interrupts & displays CT on screen):
I’ve got the CT scan for you. I will pop it up on your screen so you can read it.
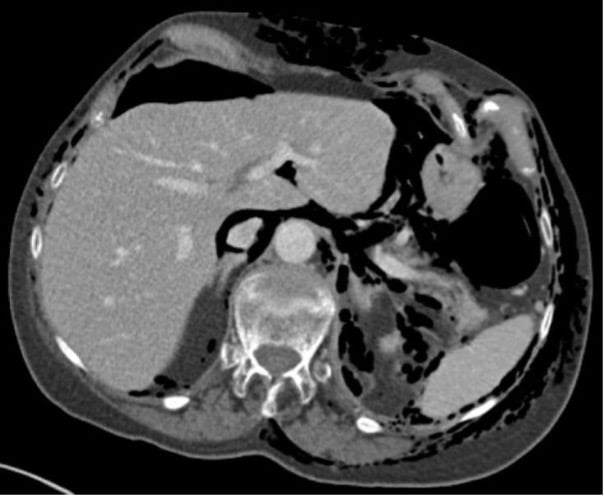
Once you’re done, we’ll discuss it further, okay?
Okay. Happy?
Candidate:
Yes.
Panellist:
From the information you’ve gathered so far, summarize for me what’s the situation with this gentleman?
Candidate:
Okay, so he has lung changes, probably chronic lung changes due to his COPD.
Panellist (interrupts):
I meant the X-ray or radiology findings in general. You’ve got all the bits and pieces you need.
Candidate:
Okay, so in general, this is a 75-year-old male who has a bowel perforation and also fecal loading in a background of comorbidity and frailty that may not be suitable for surgical intervention.
Panellist:
So what are your priorities?
Candidate:
My priorities for care would be contacting his family next of kin, having a discussion, escalating this as well to my consultant so that we can have a discussion on comfort care or end-of-life care. We’ll need to discuss with the next of kin and family with regards to RESPECT what the best interest would have been for the gentleman, given his state of mind. Also introduce palliative care, so get support from palliative care, have the patient put in a side room, put on analgesia, as well as allow for the family to come and visit.
I’d like to also support the nurses and my juniors. I’ll have an SHO there. This is a learning situation for them.
I’ll need to debrief and reflect with them about the whole situation, as well as support the nurses.
Panellist:
Okay, thank you, JW. A couple of more questions.
So you’ve made a decision that he’s not fit for surgery. So is there anybody else who could help you in coming to that conclusion?
Candidate:
Yes. So, I’d like to have a review by the anaesthetist and ITU team.
Also, I’d like to do an objective measurement, which you can do using a NELA score or a P-POSSUM score that would be able to identify the mortality risk as well as the mobility risk.
Panellist:
Okay. You’ve done all of that, and you now happen to speak to the on-call consultant to update him.
So what are you going to tell him once you’ve done all of this?
And I happen to be the on-call consultant surgeon.
Candidate:
Okay. So I have a 75-year-old male who’s a referral from a nursing home coming in with a background of several comorbidities, including COPD, ischemic heart disease, and is on an antiplatelet.
According to the investigations, he’s in sepsis, of which we’ve started treatment and resuscitation. And we have a CT scan finding that shows perforation with free air in the abdomen as well as fecal loading. The patient has dementia, and I’ve talked to the family with regards to the lack of suitability for surgery as well as I have discussed this with anaesthesia, who will review the patient and as well help with a decision on further management.
I’d like your input as to whether you agree with this treatment and if you’re available to support and come talk to the family as well. Thank you.
Panellist:
Now, just one other question.
In the patient’s records from nursing home, do you think you could get information, anything additional about his other status?
Candidate:
Yes. So I’ll check the…
Panellist (interrupts):
Don’t worry if the time runs out. Okay?
Candidate:
Okay.
I’ll check the records to see whether there’s a RESPECT FORM that has been earlier filled out.
Panellist:
Thank you. Thank you very much, JW.
Candidate:
Thank you.
Panellist:
I think there is a button on your screen you can log off.
Candidate:
Okay. Thank you.
Lastly, I’ll ensure everything is documented as well. Thanks.
Score:
| Clinical Scenario | Score out of 5 |
| Recognition of the clinical issues | 5 |
| Judgement and Prioritisation | 5 |
| Planning and use of investigations and/or resources | 5 |
| Communication strategy | 5 |
| Aggregate score: | 100% |
| Comments: 1. No concerns. 2. Needed very few prompts. 3. He has a safe approach. 4. Excellent stepwise and clear approach and management plan. 5. Covered all aspects of management, examination, and plan. | |
Detailed Feedback and Learning Points:
1. Recognition of Clinical Issues
Strengths:
- Thorough Identification: The candidate effectively identified the key clinical issues, including the patient’s acute abdominal pain, signs of sepsis, elevated lactate levels, and underlying comorbidities (COPD, dementia).
- Detailed Assessment: Recognized the potential causes for the acute abdomen such as mesenteric ischemia, perforation, or volvulus, demonstrating a comprehensive understanding of the patient’s condition.
- Holistic View: Considered the patient’s overall frailty and living conditions, ensuring a holistic approach to the case.
Weaknesses:
- Initial Complexity: While the candidate covered all aspects, the initial explanation was somewhat lengthy and complex, which could have been more concise for clarity.
- Delayed Specificity: The specific clinical details, such as the frailty score and the impact of comorbidities on treatment decisions, could have been highlighted earlier in the discussion.
2. Judgment and Prioritization
Strengths:
- Effective Prioritization: Demonstrated excellent judgment in prioritizing patient safety, initial stabilization, and the need for a multidisciplinary approach.
- Adaptability: Showed the ability to adjust priorities based on new information, such as the CT findings and the patient’s evolving clinical status.
- Clear Decision-Making: Made informed decisions about the suitability of surgical intervention versus palliative care, incorporating inputs from various specialists.
Weaknesses:
- Real-Time Adjustments: Although adaptable, the candidate’s initial response to new information (e.g., frailty assessment) could be quicker to reflect real-time clinical decision-making.
- Pressure Handling: While competent, there were moments where the candidate’s decision-making under time constraints could have been more streamlined.
3. Planning and Use of Investigations and/or Resources
Strengths:
- Comprehensive Plan: Provided a detailed and methodical plan for patient assessment, including the sepsis-6 bundle, resuscitation, and appropriate investigations (CT scan, ABGs, blood cultures).
- Multidisciplinary Involvement: Emphasized the importance of involving the consultant, anaesthetist, critical care, and palliative care teams early in the process.
- Resource Utilization: Addressed the need for communication with the radiologist for expedited imaging and with haematology regarding the patient’s antiplatelet therapy.
Weaknesses:
- Resource Awareness: Although thorough, the plan could include a more concise outline of resource allocation, particularly in a resource-limited setting.
- Sequential Approach: The sequential nature of the plan, while comprehensive, may need to be more dynamic to handle multiple concurrent issues more effectively.
4. Communication Strategy
Strengths:
- Clear Communication: Maintained clear, step-by-step communication throughout, ensuring all team members were informed and involved in the decision-making process.
- Empathy and Support: Showed empathy in discussing end-of-life care options with the family and ensuring the nursing staff and juniors were supported and debriefed.
- Structured Handover: Provided a structured and comprehensive handover to the on-call consultant, ensuring all relevant clinical details were communicated effectively.
Weaknesses:
- Conciseness: The candidate’s responses, while detailed, could benefit from being more concise to enhance clarity and efficiency in high-pressure situations.
- Proactive Updates: More proactive and regular updates to the team and family, rather than waiting for specific questions or interruptions, would further strengthen the communication strategy.
In conclusion, reviewing these real-life clinical scenario interview examples provides invaluable insights for ST3 candidates. The well-executed scenario underscores the importance of recognizing key clinical issues, demonstrating sound judgment and prioritization, methodical planning, and effective communication. Candidates can learn from the strengths and weaknesses highlighted, aiming to deliver concise, clear, and patient-centered responses. These examples emphasize the need for adaptability and proactive communication, demonstrating how the panellist with interrupt and prompt you during the interview. By reflecting on these scenarios, candidates can better prepare for their own interviews, enhancing their chances of success and improving their clinical practice.
